Scientists at Oregon State University have achieved complete cancer regression in mouse trials using a revolutionary new nanomaterial, announced January 27, 2026. The innovative treatment, detailed this week in Advanced Functional Materials, utilizes a novel iron-based metal-organic framework (MOF) to simultaneously generate both hydroxyl radicals and singlet oxygen – reactive oxygen species that destroy cancer cells while sparing healthy tissue. “When we systemically administered our nanoagent in mice bearing human breast cancer cells, it efficiently accumulated in tumors, robustly generated reactive oxygen species and completely eradicated the cancer without adverse effects,” said Olena Taratula of the OSU College of Pharmacy. This breakthrough addresses limitations of current chemodynamic therapy, offering the potential for durable therapeutic benefit and long-term prevention of recurrence, without systemic toxicity.
MOF Nanoagent Generates Both Hydroxyl & Singlet Oxygen
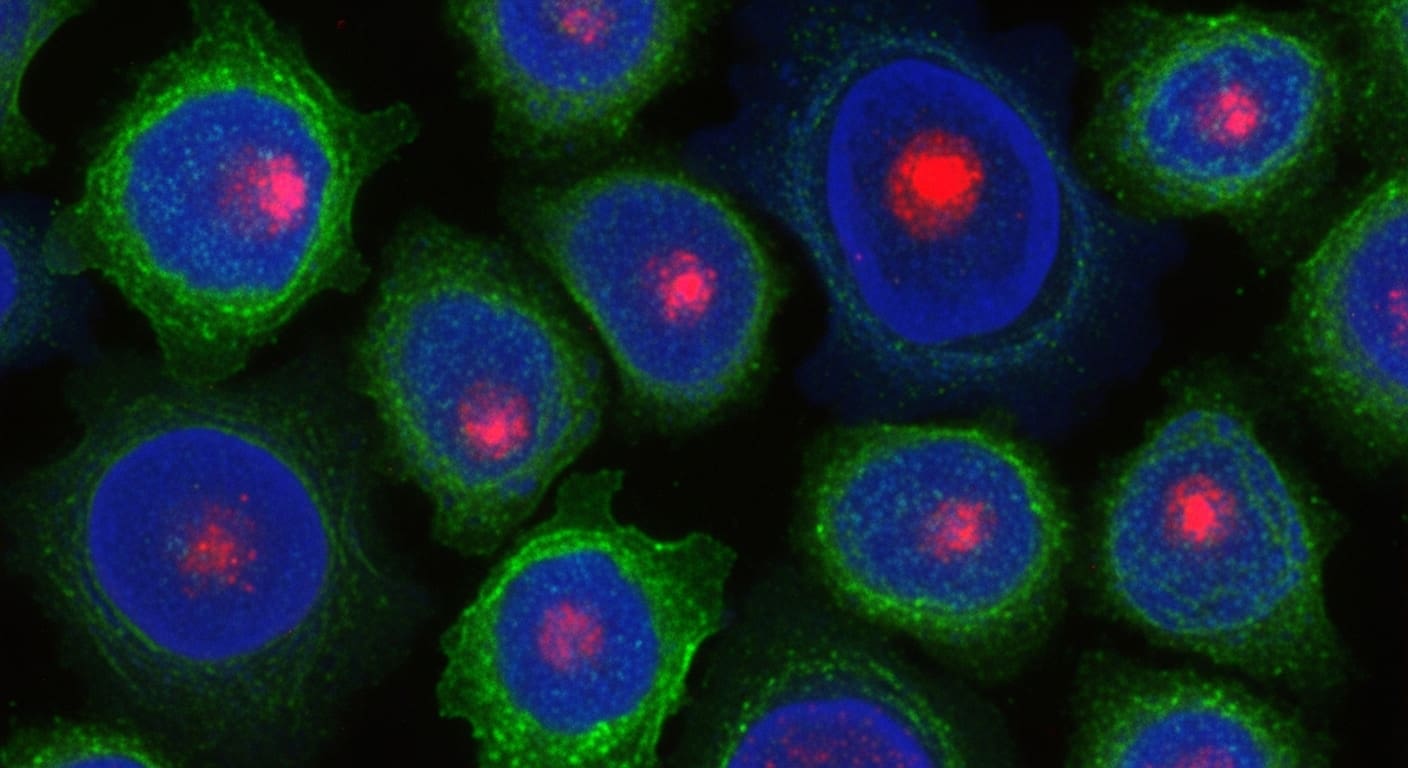
A newly developed nanomaterial from Oregon State University researchers addresses a key limitation of chemodynamic therapy (CDT) by simultaneously generating both hydroxyl radicals and singlet oxygen within cancer cells. Existing CDT agents, according to Oleh Taratula, “efficiently generate either radical hydroxyls or singlet oxygen but not both,” hindering their overall effectiveness and leading to only partial tumor regression in preclinical studies. This innovative approach utilizes an iron-based metal-organic framework (MOF) designed to maximize reactive oxygen species production, exploiting the acidic environment and high hydrogen peroxide concentrations characteristic of malignant tumors.
The MOF demonstrated significant toxicity towards multiple cancer cell lines while exhibiting “negligible harm to noncancerous cells,” a crucial safety profile. Systemic administration in mice with human breast cancer cells resulted in complete eradication of the disease and long-term recurrence prevention, as Olena Taratula explained: “We saw total tumor regression and long-term prevention of recurrence, all without seeing any systemic toxicity.” Researchers are now focused on expanding testing to other aggressive cancers, including pancreatic cancer, to assess the MOF’s broader therapeutic potential.
Tumor Microenvironment Drives Reactive Oxygen Species Production
The distinctive biochemical environment within malignant tumors is now being harnessed to amplify cancer-killing potential, according to research published January 27, 2026, in Advanced Functional Materials. Scientists discovered that tumors, unlike healthy tissues, exhibit both increased acidity and higher concentrations of hydrogen peroxide, factors crucial for a novel chemodynamic therapy (CDT) approach. Current CDT strategies typically stimulate production of either hydroxyl radicals or singlet oxygen—reactive oxygen species (ROS) that damage cancer cells—but often fall short of sustained efficacy. This new research centers on a metal-organic framework (MOF) designed to simultaneously generate both ROS types with heightened catalytic efficiency.
The team observed that systemic administration of the nanoagent in mice with human breast cancer cells led to complete tumor eradication and prevented recurrence without any detectable systemic toxicity. Further studies are planned to assess efficacy against aggressive pancreatic cancer and other malignancies.
“When we systemically administered our nanoagent in mice bearing human breast cancer cells, it efficiently accumulated in tumors, robustly generated reactive oxygen species and completely eradicated the cancer without adverse effects,” Olena Taratula said.
Olena Taratula
Complete Cancer Regression Achieved in Mouse Model
A newly developed nanomaterial demonstrated complete eradication of human breast cancer cells in a mouse model, offering a significant advancement in chemodynamic therapy (CDT). This dual-action approach addresses a key limitation of existing CDT agents, which typically produce only one type of reactive oxygen species, often resulting in “partial tumor regression and not a durable therapeutic benefit,” according to Oleh Taratula. The team, funded by the National Cancer Institute and the Eunice Kennedy Shriver National Institute of Child Health and Human Development, now intends to evaluate the therapy’s efficacy against aggressive pancreatic cancer, aiming to establish broad applicability across various malignancies.