MIT engineers have developed an implantable device capable of automatically administering glucagon. This hormone raises blood sugar, in response to dangerously low glucose levels, potentially averting life-threatening hypoglycemic episodes. Testing in diabetic mice demonstrated stabilisation of blood sugar within ten minutes of activation, and the device remained functional for up to four weeks. Funded by grants totalling over $2 million from the Helmsley Charitable Trust and the National Institutes of Health, the research aims to initiate human clinical trials within three years, offering a proactive emergency intervention for diabetes patients unable to self-administer treatment.
Automated Hypoglycemia Intervention
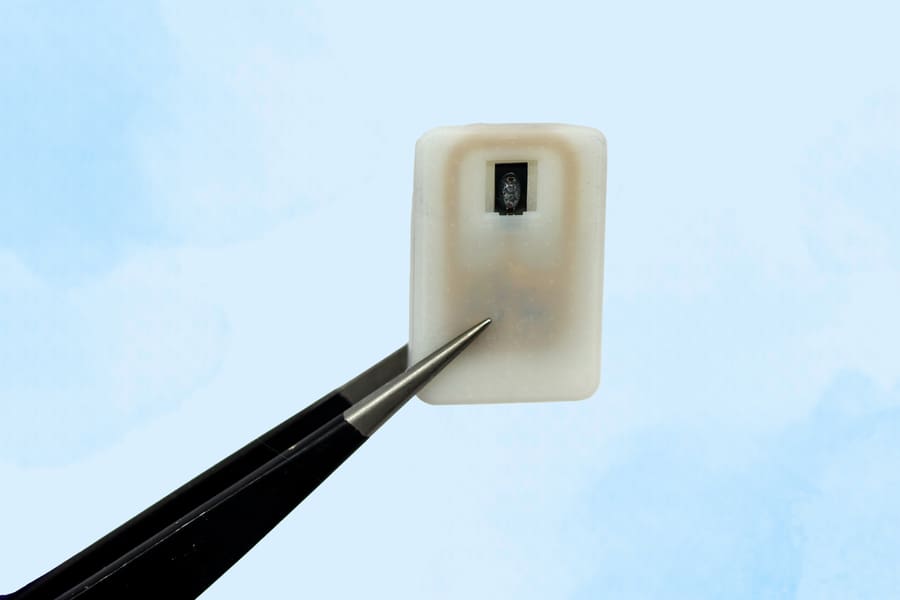
The device addresses a critical need for automated intervention in hypoglycemic events, particularly for individuals unable to self-administer glucagon. The system comprises a subcutaneous reservoir, fabricated using 3D-printing techniques, and sealed with a nickel-titanium shape-memory alloy. Activation is achieved through localised heating of the alloy to 40 degrees Celsius, inducing a conformational change that releases the stored glucagon. The formulation of glucagon as a powder ensures long-term stability within the reservoir, a key consideration for an implantable device intended for on-demand emergency use.
Crucially, the system integrates with continuous glucose monitoring (CGM) technologies. This integration enables fully automated drug delivery, triggered by predefined glucose thresholds, eliminating the need for manual activation and providing a responsive safety net. Remote activation via radiofrequency signals remains a functional capability, offering a secondary method of intervention when required.
Preclinical testing in diabetic mice demonstrated successful stabilisation of blood glucose levels within ten minutes of induced hypoglycaemia and subsequent device activation. The researchers also evaluated the device’s capacity to deliver epinephrine, observing corresponding physiological effects. While the initial functional lifespan was limited to four weeks, ongoing research focuses on extending the operational duration to several years through advancements in materials science and optimisation of biocompatibility.
Despite the inevitable formation of fibrotic tissue around the implant – a common biological response to foreign materials – consistent drug release was achieved, suggesting the device maintains functionality within the biological environment. Further animal studies are planned to refine the design and assess long-term efficacy, with a projected timeline for initiating human clinical trials within the next three years. The potential for an implantable glucagon delivery system represents a significant advancement in diabetes management, offering a proactive and automated response to a life-threatening condition.
Device Design and Functionality
The device’s physical dimensions – approximately the size of a quarter – facilitate subcutaneous implantation. The reservoir’s capacity allows for storage of either one or four doses of glucagon, providing flexibility in treatment protocols. Activation relies on a radiofrequency-responsive antenna, enabling both automated release triggered by continuous glucose monitoring data and remote, manual activation as a supplementary measure.
The use of a shape-memory alloy as the release mechanism is central to the device’s functionality. This nickel-titanium compound undergoes a predictable morphological change – from a flat configuration to a U-shape – upon reaching 40 degrees Celsius, effectively opening the reservoir and delivering the stored glucagon. This thermally induced transformation offers a precise and reliable method of drug release, independent of mechanical components that could be prone to failure.
Initial studies demonstrated sustained functionality for up to four weeks. Current research prioritises extending this operational lifespan, aiming for a device that requires replacement only after several years of implantation. This necessitates ongoing investigation into biocompatible materials and strategies to mitigate the body’s natural encapsulation response, which, while not immediately impairing function, could ultimately limit long-term drug delivery. Achieving a balance between device longevity and biological compatibility is crucial for the potential of an implantable glucagon delivery system.
Beyond glucagon, the device’s design proved adaptable to powdered epinephrine, successfully elevating blood levels and increasing heart rate in preclinical models. This suggests the platform could be extended to deliver other emergency medications, offering a versatile approach to rapid intervention in a range of critical care scenarios.
Preclinical Results and Future Development
The observed adaptability of the device to powdered epinephrine, resulting in elevated blood levels and increased heart rate in preclinical models, expands the potential applications beyond hypoglycemic events. This suggests the platform’s underlying principles could be leveraged for the delivery of other emergency medications requiring rapid systemic administration, potentially establishing a versatile system for critical care interventions.
Ongoing research prioritises extending the functional lifespan of the implant beyond the initial four-week period, with a target of several years before requiring replacement. This necessitates advancements in materials science, focusing on biocompatibility and strategies to mitigate the body’s natural encapsulation response. While the formation of fibrotic tissue around the implant did not immediately impair drug release in initial studies, long-term encapsulation could ultimately limit sustained drug delivery, demanding ongoing investigation into methods to minimise this effect.
Further animal studies are planned to refine the device design and comprehensively assess long-term efficacy and safety profiles. Successful completion of these studies will pave the way for initiation of human clinical trials, currently projected to commence within the next three years. These trials will be crucial in validating the device’s performance in a clinical setting and establishing its potential as a viable therapeutic option for individuals at risk of severe hypoglycemic episodes.
More information
External Link: Click Here For More