The American Gastroenterological Association (AGA) has released a clinical guideline on computer-aided detection (CADe) systems in colonoscopy. It concludes that while AI improves polyp detection, its impact on reducing colorectal cancer remains uncertain. Despite over 15 million annual colonoscopies in the U.S., an effective method for detecting and preventing colorectal cancer, the AGA does not currently recommend for or against widespread AI adoption.
The guideline highlights CADe’s potential to increase low-risk polyp detection without clear benefits in reducing cancer rates. Dr. Benjamin Lebwohl noted that while AI may remove more polyps, its effect on cancer incidence remains uncertain. The AGA emphasizes the need for further research to address key knowledge gaps and optimize patient outcomes.
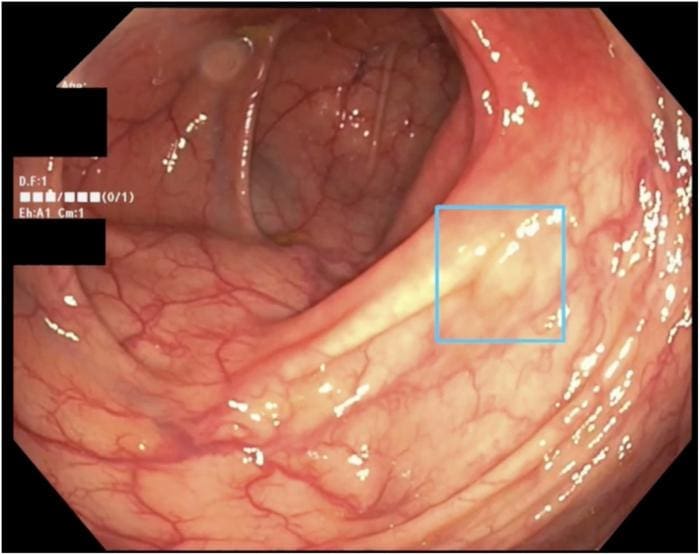
Artificial intelligence (AI) is emerging as a powerful tool in the early detection of colon cancer. By leveraging advanced algorithms, AI systems can analyze medical images highly, potentially improving diagnostic accuracy and reducing the risk of missed detections. This technology holds significant promise for enhancing patient outcomes by enabling earlier intervention.
The American Gastroenterological Association (AGA) has issued a living clinical practice guideline on AI-driven colonoscopy, acknowledging the potential benefits of AI in improving lesion detection during colorectal cancer screening. The guideline highlights that AI systems can enhance the identification of precancerous polyps compared to traditional methods. However, it also emphasizes insufficient evidence to recommend routine use of these systems due to gaps in understanding their long-term outcomes.
Integrating AI into clinical practice presents several challenges, including cost considerations, the need for specialized training, and the establishment of standardized metrics to evaluate system performance across different studies and populations. While AI shows promise in improving diagnostic accuracy and efficiency, more research is needed to confirm its effectiveness in real-world settings.
Experts express cautious optimism about the adoption of AI in colorectal cancer screening. They acknowledge that AI systems have demonstrated improved lesion detection rates during colonoscopy, which could enhance early identification of precancerous polyps. However, they also stress the need for further studies to establish whether these technologies can significantly reduce cancer incidence and mortality.
The AGA’s guideline underscores several key knowledge gaps that require further investigation. These include understanding the long-term impact of AI systems on patient outcomes, determining their cost-effectiveness, and developing standardized evaluation metrics to assess performance across different clinical settings. Addressing these gaps will be crucial for optimizing the role of AI in colorectal cancer screening.
The AGA’s living guideline reflects a dynamic approach to clinical recommendations, allowing for updates as new evidence emerges. This ensures that clinicians can access the most current information while balancing the potential benefits and uncertainties associated with AI-driven diagnostic tools. As CADe systems continue to evolve, their role in optimizing colorectal cancer screening will depend on rigorous evaluation of both diagnostic performance and broader public health impacts.
More information
External Link: Click Here For More